Partnerships in healthcare can align and become highly beneficial to the most vulnerable among us, offering advanced care plans amid a strong and cooperative atmosphere. To improve the healthcare of newborn patients and the ability to treat premature newborns, PeaceHealth St. Joseph Medical Center is entering an exciting collaboration with Seattle Children’s Hospital — along with massive preparations for the partnership in the childbirth center. Nurse Manager Gallit Eni, Pediatric Hospitalist and Medical Director for pediatrics Dr. Mara Kelley, and Pediatric Hospitalist and Associate Medical Director over newborn medicine Dr. Brooke Jardine sat down with WhatcomTalk to discuss PeaceHealth St. Joseph’s brand-new directive in union with Seattle Children’s Hospital.
“We are currently licensed to a special care nursery, but we’ve been operating as a modified special care nursery,” says Eni. “We have always taken care of patients of any gestation but those babies that are less than 34 weeks are transferred out to a higher level of care. Now, with the collaboration, we will have the ability to care for sicker babies.”

PeaceHealth St. Joseph’s labor and delivery unit has always had a solid connection with Seattle Children’s Hospital when it involves a patient with higher care needs. Now, they can put that partnership in writing while vastly improving the quality of life for community patients.
“We’ll be able to keep patients within our community and care for our patients at PeaceHealth,” Eni says. “We’re still not going to be able to keep all babies, but we’ll be able to care for them and transfer them if they’re less than 32 weeks. With this collaboration, we can care for babies 32 weeks and above, versus 34 weeks and above.”
To reach this goal, PeaceHealth St. Joseph’s has been extremely busy, planning each step of preparation with great detail and care.
“It’s been quite a ride,” says Eni. Preparing and caring for 32-week-old babies doesn’t just include the hard work of nursing and provider staff. “We’ve been collaborating with the whole hospital.”
The pharmacy provides different medications necessary for babies born a little earlier. Respiratory therapists help babies that may need more respiratory assistance. The nutrition unit assists babies that need a different type of help than is typically offered by other staff nutritionists. Even the obstetricians are part of the collaboration because they, of course, care for the mother of the newborn baby.
As pediatric hospitalists, Dr. Jardine and Dr. Kelley work to perfect a newborn’s care from every angle. Both are excited to bring the partnership with Seattle Children’s to life.

“We’ve had a strong pediatric presence for years at St. Joseph’s Medical Center with really committed doctors, amazing special care unit nurses, and respiratory therapists,” says Dr. Kelley. “We are always looking, as pediatricians, at how to optimize care in our community.”
The goal is to avoid families having to travel south for premature newborn care and to optimize what our local hospital can do. The partnership with Seattle Children’s Hospital does just that. “We are going to grow a level two special care nursery and afford our birth parents the opportunity to live in their community, care for their families at home, and also be really present for their babies during this time,” Dr. Kelley says.

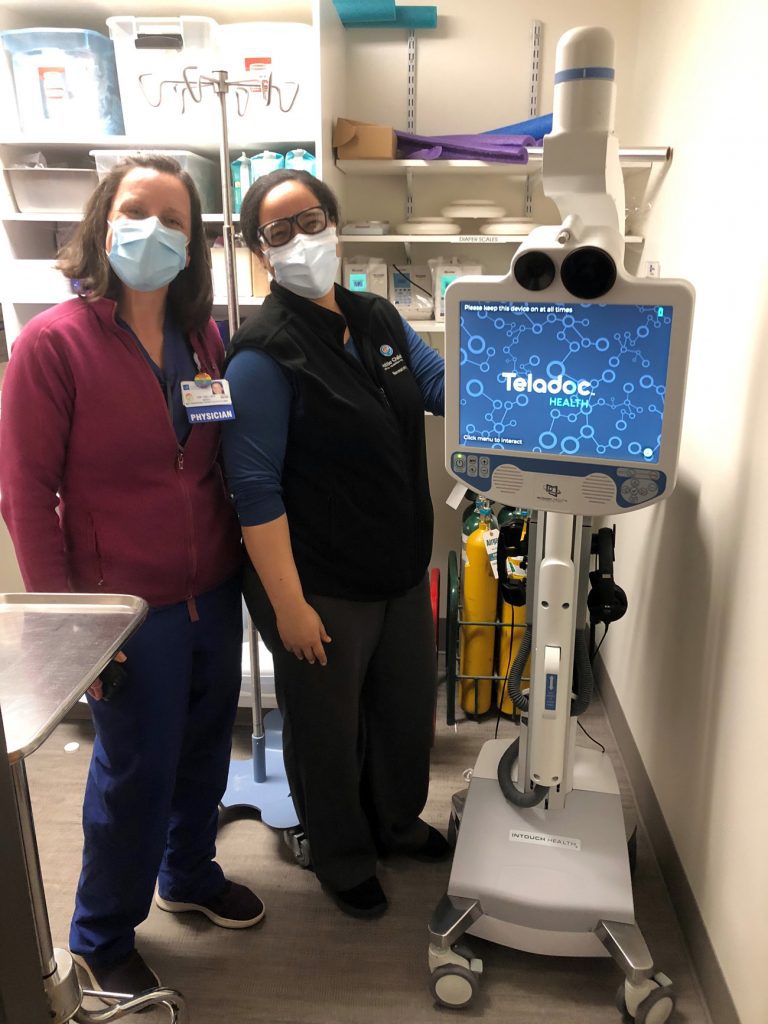
There are two main components to the improved healthcare in this collaboration: neonatology with telehealth and telerounding. “By Department of Health regulations, we have to have a neonatologist to be able to achieve this new level of care,” says Dr. Kelley, “Neonatologist Dr. Hedstrom has been assigned to us and she spends a lot of time with us doing pathway development, with policy development, and also virtual and hands-on education.”
With the aid of a specially designed device, an on-call neonatologist for telehealth can join providers on a resuscitation or stabilization, treatment involving a newborn right after birth, and ensuring the safety and preparedness of a newborn until they require transportation.

“Telerounding will grant us the opportunity to go from bedside to bedside a couple times a week,” Dr. Kelley says. “We will be able to talk about how each baby is doing and make sure we have an interdisciplinary look at each baby’s healthcare needs.”
One of the most important aspects to improved newborn care is a critical examination of their nutritional needs in conjunction with other — still developing, yet critical — bodily functions.
“This is going to allow us to keep babies that are eight weeks premature, and a lot of the services those babies need we are already providing,” says Dr. Jardine. “The main things these babies potentially need are increased support for their nutrition, their temperature regulation, and their respiratory support. We have several new protocols, pathways, and plans of care. We’ve really looked into the nutritional needs for these babies in terms of calories and some of the other necessary nutrients they need to develop clear plans for their overall nourishment.”
Dr. Jardine also praises another recent development of PeaceHealth St. Joseph’s in relation to newborn nourishment: a donor breastmilk program. “We now have a donor breastmilk program where patients can receive donor breastmilk until parents can produce enough of their own breastmilk,” Dr. Jardine says. “This has been in place since January.”
When the collaboration goes live, patients can expect a new dimension to an already robust healthcare fellowship between PeaceHealth St. Joseph Medical Center and Seattle Children’s Hospital, an outstanding achievement for the staff PeaceHealth St. Joseph in Bellingham.
Sponsored